Powassan Virus
Powassan virus (POWV) is part of the Flaviviridae family, similar to West Nile, Zika, and Dengue virus. Flaviviruses are enveloped and RNA viruses that are mainly transmitted by ticks or mosquitos1. POWV belongs to the tick-borne encephalitis (TBE) complex, which is a group of viruses that are genetically similar and can cause severe encephalitis (inflammation of the brain), meningitis (inflammation of the brain and spinal cord), and/or hemorrhagic fevers in humans2. There are two groups of POWV arising due to differences in their genome sequence: lineage I called POWV and lineage II called deer tick virus (DTV)3, both linked to human disease (Figure 1). The name of this virus comes from the place where it was first identified. POWV was isolated from the brain of a five-year-old boy who died of encephalitis in the town of Powassan, Ontario in 19584 (Figure 1).
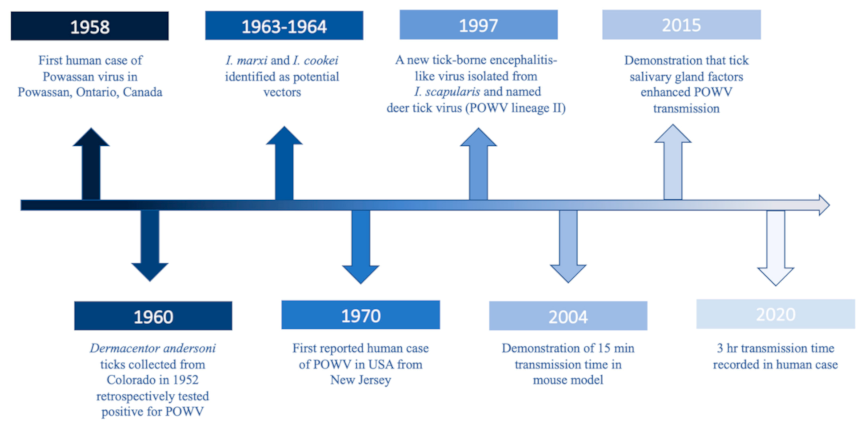
Figure 1: Timeline of major Powassan virus milestones from Hassett and Thangamani, 20213
Transmission, Clinical Symptoms and Disease
POWV is carried by ticks and transmitted through their bites to humans, similar to Lyme disease. In North America, POWV is transmitted by Deer tick (Ixodes scapularis) and Groundhog tick (Ixodes cookei). Ticks live in shady, moist areas at ground level. Ticks cling to tall grass, brush, and shrubs waiting for their next animal or human host. POWV transmission time is 15 minutes after tick attachment, much shorter than in Lyme disease that takes from 36 to 48 hours5-7.
Interestingly, infected people do not develop a rash after the tick bite in contrary to other tick-borne diseases and many infected people remain asymptomatic. In symptomatic cases, people develop symptoms such as fever, headache, and sometimes altered consciousness from approximately 1 week to 1 month after the tick bite 8. The virus thereafter can infect the brain causing inflammation resulting in loss of breath, coordination, speech, and ultimately paralysis and seizures9,10. Approximately 1 in 10 people with severe disease succumb to death and half of POWV survivors have permanent neurological damage 5. In the past 10 years, 21 people have lost their lives because of POWV 11.
Treatment of POWV
Currently, there is no vaccine or specific treatment available, but only supportive care to manage and alleviate the symptoms8. Pharma companies and research institutes are working on developing a successful vaccine 12,13. The best way to prevent POWV disease is to protect yourself from tick bites by 1) avoiding tall grass and overgrown areas 2) wearing long sleeves, long pants tucked into socks, and shoes 3) using insect repellent 4) performing tick checks after coming in from the outdoors14.
Countries Affected
POWV infection in humans has been documented in the United States (U.S.), Canada, and Russia (Figure 2). POWV human cases have to be reported to the state’s public health labs in the U.S. since 2001 for neuroinvasive infection (infecting the brain and spinal cord) and in 2004 as non-neuroinvasive (mild symptoms without infecting the brain and spinal cord). The majority of the infections are being reported from Northeastern and Midwestern states where there is a high prevalence of Deer tick (Ixodes scapularis), and Groundhog tick, (Ixodes cookei) 11.

Figure 2: Approximate distribution of Powassan virus in North America. Adapted from Lindqvist et al. 2018 15
Rate of POWV Infection
The prevalence of POWV infection is lower compared to other tick-borne disease infections. Primarily this is because majority of the patients who are infected remain asymptomatic. Secondly, many of the labs in the U.S. and Canada do not even test for POWV16. Nevertheless, the number of documented POWV infections in humans has been increasing over the years. In the last ten years, 186 human cases of POWV infection have been reported in the U.S11 and 17 cases in Canada since 201717.
Diagnosis of POWV Infection
POWV infection is diagnosed based on clinical symptoms and history of possible exposure to the aforementioned ticks. Laboratory testing of blood or cerebrospinal fluid (CSF) is used to support the diagnosis of POWV infection7.
Molecular tests to detect the virus in the blood and CSF are used for the detection of the early phase of the infection. Positive results indicate presence of POWV infection. However, negative results do not indicate lack of infection because the virus persists in the blood and CSF only for a short period of time, while the disease progresses. Therefore, negative results of patients with suspicion of POWV infection have to be confirmed with serologic results to detect antibodies such as IgM and IgG. As mentioned above there are two genetically different groups (lineages) of POWV. However, based on antibody detection these two groups are indistinguishable3. A positive antibody test has to be confirmed by neutralizing antibody testing (plaque reduction neutralization test (PRNT)). Immunoassays and PRNT to detect antibodies against POWV are available by the state’s public health labs as well as the CDC7.
Future Perspectives
The number of POWV reported cases is low compared to other tick-borne diseases such as Lyme disease. However, the prevalence of POWV infection is likely underestimated because testing capabilities are limited. There are no FDA-cleared assays and only a few commercially available assays. There is a need to increase the awareness of POWV infection to include this testing in clinical routine labs. It would be also beneficial to educate the population in endemic areas to minimize exposure to ticks. To learn more about Powassan virus, click here and join our webinar on emerging tick-borne diseases on December 14th at 11 am. Register here
References
- Mrozowich T, Henrickson A, Demeler B, Patel TR. Nanoscale Structure Determination of Murray Valley Encephalitis and Powassan Virus Non-Coding RNAs. Viruses. 2020;12(2):190.
- McAuley AJ, Sawatsky B, Ksiazek T, et al. Cross-neutralisation of viruses of the tick-borne encephalitis complex following tick-borne encephalitis vaccination and/or infection. NPJ Vaccines. 2017;2:5.
- Hassett EM, Thangamani S. Ecology of Powassan Virus in the United States. Microorganisms. 2021;9(11):2317.
- McLean D, Donohue WL. Powassan virus: isolation of virus from a fatal case of encephalitis. Can Med Assoc J. 1959;80(9):708-711.
- Hermance ME, Thangamani S. Powassan Virus: An Emerging Arbovirus of Public Health Concern in North America. Vector Borne Zoonotic Dis. 2017;17(7):453-462.
- Frost H, Schotthoefer A, Thomm A, et al. Serologic Evidence of Powassan Virus Infection in Patients with Suspected Lyme Disease. Emerging Infectious Disease journal. 2017;23(8):1384.
- CDC. Powassan: Diagnostic Testing https://www.cdc.gov/powassan/diagnostic-testing.html. Accessed November 11, 2021.
- CDC. Powassan virus: Symptoms, Diagnosis, and Treatment. https://www.cdc.gov/powassan/symptoms.html. Accessed November 11, 2021.
- Neitzel DF, Lynfield R, Smith K. Powassan virus encephalitis, Minnesota, USA. Emerg Infect Dis. 2013;19(4):686-686.
- Piantadosi A, Rubin DB, McQuillen DP, et al. Emerging Cases of Powassan Virus Encephalitis in New England: Clinical Presentation, Imaging, and Review of the Literature. Clin Infect Dis. 2016;62(6):707-713.
- CDC. Powassan virus: Statistics & Maps. https://www.cdc.gov/powassan/statistics.html. Accessed November 11, 2021.
- Cimica V, Saleem S, Matuczinski E, et al. A Virus-Like Particle-Based Vaccine Candidate against the Tick-Borne Powassan Virus Induces Neutralizing Antibodies in a Mouse Model. Pathogens. 2021;10(6).
- VanBlargan LA, Himansu S, Foreman BM, Ebel GD, Pierson TC, Diamond MS. An mRNA Vaccine Protects Mice against Multiple Tick-Transmitted Flavivirus Infections. Cell Rep. 2018;25(12):3382-3392.e3383.
- CDC. Preventing tick bites https://www.cdc.gov/ticks/avoid/on_people.html. Published 2020. Updated 2020-07-01T01:58:08Z. Accessed November 14, 2021.
- Lindqvist R, Upadhyay A, Överby AK. Tick-Borne Flaviviruses and the Type I Interferon Response. Viruses. 2018;10(7):340.
- Fatmi SS, Zehra R, Carpenter DO. Powassan Virus—A New Reemerging Tick-Borne Disease. Frontiers in Public Health. 2017;5(342).
- Canada National collaborating center for infectious diseases Powassan Virus. https://nccid.ca/debrief/powassan-virus/. Accessed November 14, 2021.