Testosterone is a hormone produced in the reproductive organs of people assigned both male and female at birth (yes, females too!). Although testosterone is mainly produced in the testes and ovaries for those assigned male and female at birth, respectively, smaller amounts are synthesized in the adrenal glands.1 While testosterone is an androgen, a hormone defined as stimulating the development and maintenance of male sex characteristics, it also influences various processes in all humans. Although testosterone’s physiological role is better understood in the context of males, we know that most, but not all testosterone is converted to estrogen in females.2 Nonetheless, testosterone is vital for maintaining muscle mass, bone density, and libido in all people, making it essential for overall health no matter if you were born male or female.3
Now that we know testosterone is important in all genders, let’s break it down even further:
In those assigned male at birth, testosterone supports1,2:
- Development of secondary sex characteristics during puberty (i.e. deepening of the voice, increased body hair)
- Sperm production, fertility, and libido
- Maintaining muscle mass and strength
- Bone density and strength
- Cardiovascular health4
- Metabolism and mood
In those assigned female at birth, testosterone contributes to1,2:
- Proper ovarian function, fertility, and libido
- Muscle mass and strength
- Bone density and strength
- Cardiovascular health4
- Metabolism and mood
Most of the testosterone in our blood (up to 99%!) is bound up by proteins—particularly sex hormone-binding globulin (SHBG) (60-80%) and albumin (20-40%).3 The portion of testosterone bound to SHBG is thought to be inactive due to their strong chemical interaction, while albumin-bound testosterone can dissociate and is considered mildly active and bioavailable (Figure 1). You can think of this bound up testosterone as cash locked in a safe or money in your savings account, you cannot access it immediately.
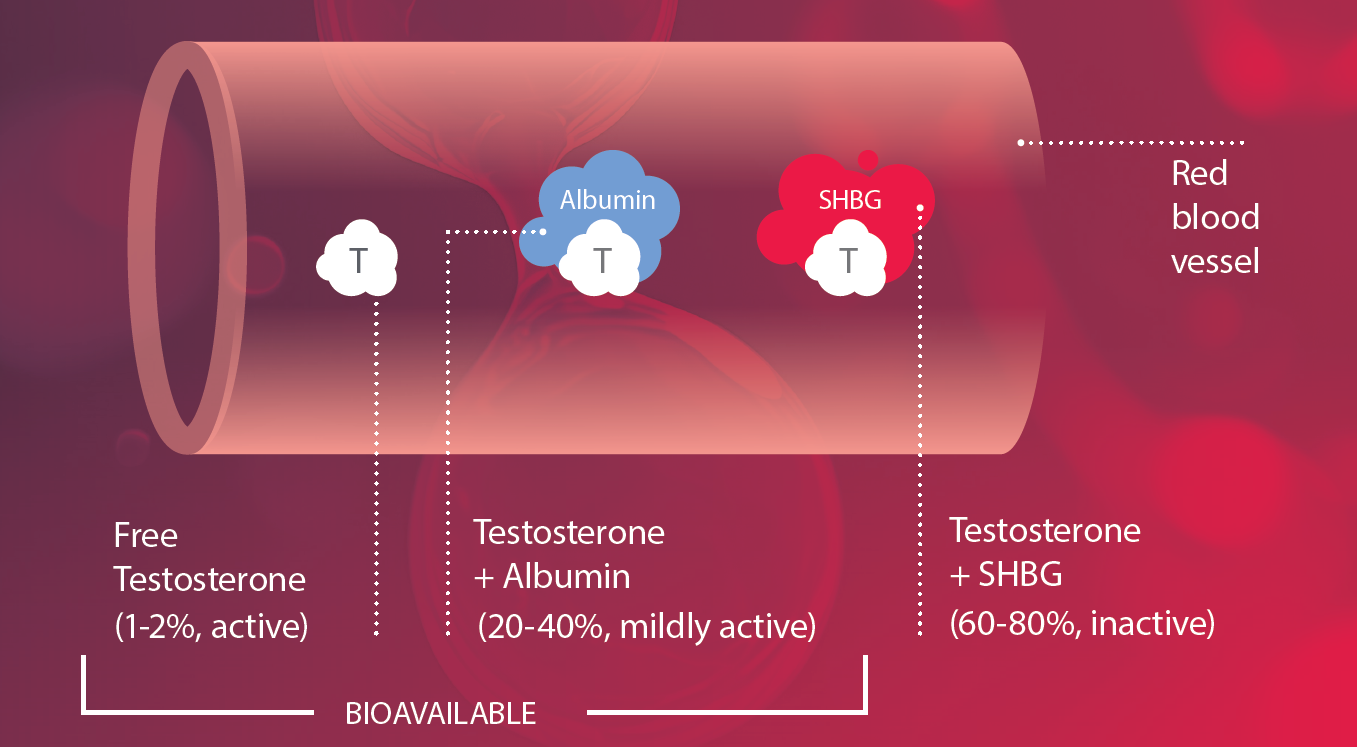
Figure 1. Total testosterone illustrated as the combination of free testosterone, albumin-bound, and SHBG-bound testosterone.
More importantly, there is a small percentage (1‒2%) of testosterone that floats freely in our blood, and we call this (not surprisingly) free testosterone. Free testosterone is readily (bio)available to bind tissues throughout the body and is the form that actively influences the processes mentioned above. Think of free testosterone as the cash in your wallet, ready instantly—although in much smaller quantities—to purchase that morning cup of coffee that keeps you going.
So, what happens when our testosterone levels aren’t within range?
Levels that are either too high or too low are related to various disorders in those assigned both male and female at birth and during all stages of life from in utero to adolescence to late-adulthood.1 It is even thought that testosterone might play a role in other endocrine or metabolic disorders such as obesity, diabetes, and cardiovascular disease.2,3 Here we will briefly discuss the most common disorders associated with altered testosterone levels.
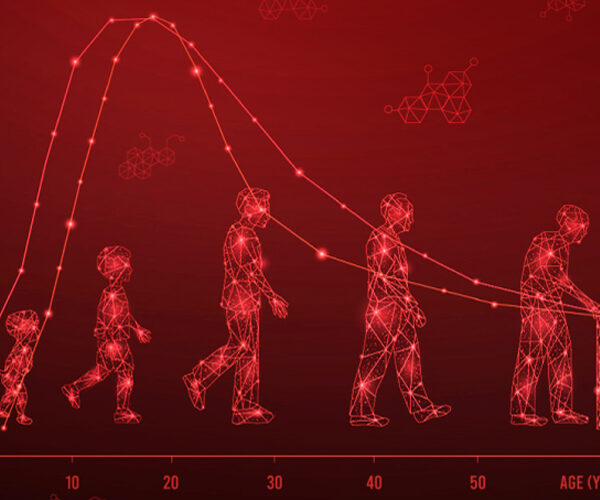
Disorders of androgen deficiency (i.e. hypogonadism5) occurs when the body is not producing sufficient testosterone, affecting approximately 2% of men, with the risk increasing with age. For men, testosterone peaks in the third decade of life and then begins a gradual decline. Symptoms include fatigue, reduced muscle mass, decreased bone density, mood changes, and low libido. These men are also at risk for bone-related issues, like osteoperosis.3,6
Disorders of androgen excess (i.e. hyperandrogenism7) are commonly associated with PCOS where there is an excess production of testosterone in women. This affects 10-13% of reproductive-aged women, globally. Symptoms include excess body hair, acne, weight gain, male-pattern baldness, irregular menses, and infertility.8
For diagnosing these disorders, in addition to monitoring hormone therapies, clinicians like to have an idea about testosterone levels, with free testosterone being particularly relevant in women due to their physiologically low concentrations.8 While total testosterone can provide a broad picture, free testosterone may offer a more precise measure of the hormone’s activity in the body.
Free testosterone is the most sensitive test for hyperandrogenemia in women8, but guidelines for hypogonadism in men6 only currently require total testosterone measurements. Importantly, free testosterone is vital in cases of suspected hypogonadism where total testosterone is borderline or SHBG concentrations are skewed, since methods to calculate free testosterone are dependent on SHBG. Importantly, SHBG concentration can be contingent on factors such as diet, body mass index (BMI), insulin, thyroid and sex hormone concentrations, and age6—making free testosterone measurements essential when male patients present with secondary metabolic disorders such as diabetes or infections such as HIV. Not to mention, total testosterone varies considerably from person to person and between age groups.1,9
A case study…
Picture a woman in her mid-late twenties trying to conceive with their partner. They are disappointed by consistently negative pregnancy tests for almost a year. Suddenly, her irregular periods make it difficult to plan pregnancy, although this has never presented as a major issue before. The thinning hair on her head has seemed like a product of aging as her 30s approached. She gained weight during college and has had trouble shedding it since, but all bodies are different. And the thick hair on her body had never been a problem due to accessibility of modern-day hair removal methods. But after continued frustration and trouble conceiving, they see a doctor who upon examination suspects PCOS due to a high BMI, moderate hirsutism (excess hair), yet normal total testosterone and elevated free testosterone levels, which is potentially contributing to the infertility issues. Her and her doctor can now work together to make informed decisions about pregnancy, since she is now considered high risk8, while seeking solutions such as lifestyle changes.
Note: This case, although based on an actual case study10, is fictional, and intended for educational purposes, only.
Testing for free testosterone is a simple yet powerful tool that can help corroborate clinical symptoms, especially in the 20-40% of women who fall within the reference range for total testosterone, yet experience clinical symptoms of androgen excess.3 These naturally low levels in women challenge the limited sensitivity and accuracy of some total testosterone assays, highlighting the limitations of total testosterone testing, along with the utility of free testosterone in certain populations.
Measuring Free Testosterone Levels
The gold standard for measuring free testosterone in the blood is a method called equilibrium dialysis (ED) followed by liquid chromatography and mass spectrometry (LCMS). This method first uses a porous membrane to restrict the movement of the larger, SHBG- and albumin-bound testosterone and then separates other unwanted impurities to detect only unbound, free testosterone. While this method can detect the low levels of free testosterone often present in women and children, it is expensive, time-consuming, and requires technical expertise. Additionally, free testosterone can be calculated, indirectly, via concentrations of total testosterone, SHBG, and albumin using the Vermeulen equation. While convenient, this method also has its drawbacks, with studies showing up to a 30% overestimation11 of free testosterone when calculations are used. To further complicate things, total testosterone concentrations depend on SHBG, which if you recall from earlier, is often skewed in patients with comorbidities like infection or metabolic disorders.6
Radioimmunoassay (RIA) and ELISA can also be used to measure free testosterone, but these methods are not appropriate for women or children due to their low sensitivity and inconsistent results.12 Emerging methods like chemiluminescent assays (ChLIA) might be a more time-efficient, cost-effective, and reproducible approach.
Our bodies tightly regulate testosterone levels, regardless of whether we are born male or female. Accurate and appropriate testing for both total and free testosterone is essential to monitor treatment or support confidence in clinical symptoms when concentrations fall outside the range deemed acceptable by your physician.
References:
1 Cleveland Clinic. Testosterone, <https://my.clevelandclinic.org/health/articles/24101-testosterone> (2022).
2 Bianchi, V. E. et al. The role of androgens in women’s health and wellbeing. Pharmacol Res 171, 105758, doi:10.1016/j.phrs.2021.105758 (2021).
3 Shea, J. L., Wong, P. Y. & Chen, Y. Free testosterone: clinical utility and important analytical aspects of measurement. Adv Clin Chem 63, 59-84, doi:10.1016/b978-0-12-800094-6.00002-9 (2014).
4 Bianchi, V. E. Testosterone, myocardial function, and mortality. Heart Fail Rev 23, 773-788, doi:10.1007/s10741-018-9721-0 (2018).
5 Cleveland Clinic. Low Testosterone (Male Hypogonadism), <https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism> (2022).
6 Jayasena, C. N. et al. Society for Endocrinology guidelines for testosterone replacement therapy in male hypogonadism. Clin Endocrinol (Oxf) 96, 200-219, doi:10.1111/cen.14633 (2022).
7 Cleveland Clinic. Hyperandrogenism, <https://my.clevelandclinic.org/health/diseases/24639-hyperandrogenism> (2023).
8 Teede, H. J. et al. Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Fertil Steril 120, 767-793, doi:10.1016/j.fertnstert.2023.07.025 (2023).
9 Jasuja, R. et al. Reference intervals for free testosterone in adult men measured using a standardized equilibrium dialysis procedure. Andrology 11, 125-133, doi:10.1111/andr.13310 (2023).
10 McCartney, C. R. & Marshall, J. C. CLINICAL PRACTICE. Polycystic Ovary Syndrome. N Engl J Med 375, 54-64, doi:10.1056/NEJMcp1514916 (2016).
11 Fiers, T. et al. Reassessing Free-Testosterone Calculation by Liquid Chromatography-Tandem Mass Spectrometry Direct Equilibrium Dialysis. J Clin Endocrinol Metab 103, 2167-2174, doi:10.1210/jc.2017-02360 (2018).
12 Bhasin, S. et al. Testosterone Therapy in Men With Hypogonadism: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab 103(5): 1715-1744. doi: 10.1210/jc.2018-00229