Autoimmune liver diseases (ALD) occur when the immune system turns against liver cells, leading to inflammation. More specifically, ALDs are characterized by the production of autoantibodies against the liver. Types of ALD include autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC). The detection of specific disease-associated antibodies allows for a differential diagnosis of the culprit ALD, in addition to helping rule out other possible causes of a patients’ symptoms. It is important to distinguish between different ALD because the treatment for one disease differs from that of another. Here we discuss the specific autoantibodies associated with either AIH, PBC, or PSC, as well as the techniques available for their detection.
Autoimmune Hepatitis
AIH mainly affects women (75% of cases) and manifests as an increase in bilirubin, an orange-yellow pigment formed in the liver by the breakdown of hemoglobin, and increases in liver enzymes, and immunoglobulin G (IgG) levels.1 The prevalence of AIH In North American populations is estimated as ∼1 in 100,000 people.2 If untreated, AIH develops into liver scarring (cirrhosis) which is life threatening. However, with treatment that suppresses the immune system, called immunotherapy, patients can have a normal life expectancy.3 The detection of circulating antibodies in AIH plays an important role in AIH diagnosis. The detection of antibodies allows for a differential diagnosis of AIH, helping to rule out potential hepatitis viral infection.4 AIH is associated with several autoantibodies including those against cell nuclei (ANA), native DNA, smooth muscle, soluble liver antigen/ liver-pancreas antigen (SLA/LP), liver-kidney microsomes (LKM-1) and liver cytosolic antigen type 1 (LC-1).4
The detection of autoantibodies against SLA/LP provides the highest diagnostic accuracy of all the AIH-associated antibodies. The predictive value of autoantibodies against SLP/LP is close to 100%, meaning that if they are detected in a patient with corresponding clinical symptoms of AIH, a definitive diagnosis of AIH can be made.5 Antibodies against smooth muscle (SMA) also indicate AIH and is a requites for the diagnosis of AIH.4 In typical cases of AIH, a high number of SMA are detected.
Primary Biliary Cirrhosis
PBC is a an immune-mediated liver disease that occurs when the liver biliary ducts are destroyed by the body’s immune system. This leads to a decrease in bile flow resulting in bile buildup (cholestasis). PBC occurs predominantly in females (>90% of cases) and is commonly characterized by fatigue and itchy skin.6 If untreated, PBC can lead to liver cirrhosis and ultimately liver failure (Figure 1). Other organs with exocrine functions can also be affected, including the lachrymal and salivary glands and the pancreas.
The diagnosis of PBC involves liver function tests (alkaline phosphatase, aspartate transaminase and alanine transaminase), the finding of histological features characteristic of PBC in liver biopsy, and the presence of PBC-specific antibodies (specifically antibodies against mitochondria (AMA)). The additional determination of ANA is recommended, in particular antibodies against nuclear dots (Sp100 und PML) and nuclear membrane (gp210). Anti-gp210 antibodies are found in 50% of patients that are negative for AMA.7 Therefore, it is important to screen for both AMA and ANA.
The detection of antimitochondrial antibodies (AMA) in PBC patients is a useful diagnostic tool as they are found in the serum of 90% of patients affected.8 Antibodies that are directed M2 component of the mitochondria represent the most sensitive and specific diagnostic marker for PBC. A positive detection of anti-M2 antibodies is also a powerful predictor of PBC development in patients without symptoms.
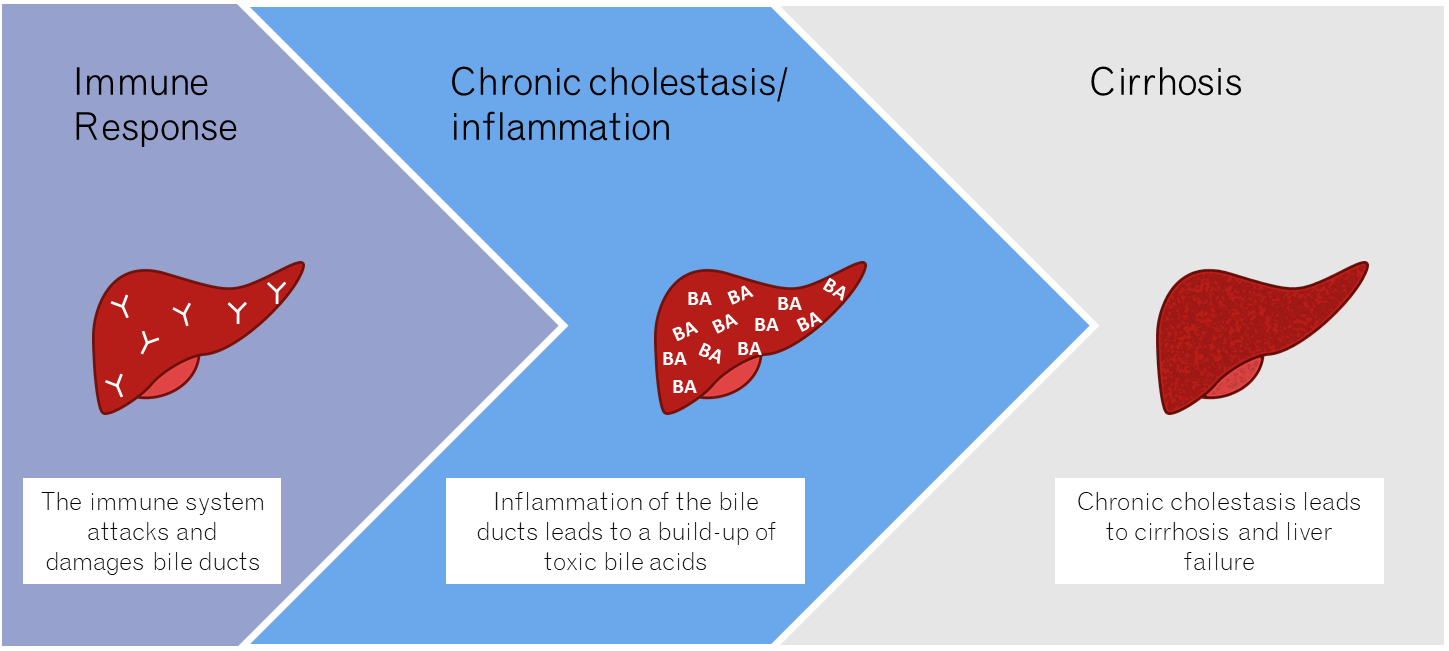
Figure 1. PBC occurs as a result of an autoimmune response against the liver. If untreated, cholestasis leads to liver scarring (cirrhosis) and ultimately liver failure.
PBC and AIH overlap syndrome
Certain cases of overlap of AIH with PBC have been reported, and up to 10% of AIH or PBC patients may belong in this overlap category.8 Because ANA are found in both AIH and PBC patients, they do not represent a helpful marker of overlap syndrome. Additionally, the presence of SLA/LP in PBC patients does not appear to be related to AIH overlap. One study however, concluded that SMA positivity in PBC patient is correlated with AIH overlap.9 Antibodies against centromere proteins are found regularly in a proportion of PBC patients with overlap syndrome with systemic sclerosis.
Primary sclerosing cholangitis
PSC is a chronic choleastic liver disease characterized by the progressive destruction of the liver bile ducts. PSC occurs twice as often in men than in woman. The disease prevalence is about 8-14 patients in 100,000 people. PSC occurs in patients with chronic inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease. Cholangiography-an X-ray examination of the bile ducts is the diagnostic gold standard for PSC. However, most patients with PSC also exhibit antibodies against antineutrophilic antibodies (ANCA). ANCA can also be found in AIH patients who are negative for conventional AIH antibodies.
Key Takeaways
The identification of autoantibodies in ALD is important for an accurate and reliable diagnosis. An accurate diagnosis is needed for proper patient treatment, as different liver diseases require different therapies. In addition, earlier treatment increases survival in those with ALD.
References
- Gatselis NK, Zachou K, Koukoulis GK, Dalekos GN. Autoimmune hepatitis, one disease with many faces: etiopathogenetic, clinico-laboratory and histological characteristics. World J Gastroenterol. 2015;21(1):60-83.
- Boberg KM. Prevalence and epidemiology of autoimmune hepatitis. Clinics in liver disease. 2002;6(3):635-647.
- Kanzler S, Löhr H, Gerken G, Galle PR, Lohse AW. Long-term management and prognosis of autoimmune hepatitis (AIH): A single center experience. Z Gastroenterol. 2001;39(05):339-348.
- Zachou K, Rigopoulou E, Dalekos GN. Autoantibodies and autoantigens in autoimmune hepatitis: important tools in clinical practice and to study pathogenesis of the disease. J Autoimmune Dis. 2004;1(1):2-2.
- Zhao Y, Yan HP, Tan YF, et al. [The significance of anti-soluble liver antigen/liver-pancreas in diagnosing and typing autoimmune hepatitis]. Zhonghua Gan Zang Bing Za Zhi. 2007;15(4):283-286.
- Swhr. @SWHR. https://swhr.org/9-in-10-people-with-this-rare-liver-disease-are-women/. Published 2020. Updated 2020-09-08. Accessed.
- ITOH S, ICHIDA T, YOSHIDA T, et al. Autoantibodies against a 210kDa glycoprotein of the nuclear pore complex as a prognostic marker in patients with primary biliary cirrhosis. Journal of gastroenterology and hepatology. 1998;13(3):257-265.
- Washington MK. Autoimmune liver disease: overlap and outliers. Modern Pathology. 2007;20(1):S15-S30.
- Chazouillères O, Wendum D, Serfaty L, Montembault S, Rosmorduc O, Poupon R. Primary biliary cirrhosis–autoimmune hepatitis overlap syndrome: Clinical features and response to therapy. Hepatology. 1998;28(2):296-301.