Two well-known growth hormone (GH) disorders are GH deficiency and GH excess: gigantism in children and acromegaly in adults. These are rare diseases.
GH deficiency occurs when the pituitary does not make enough GH and can happen at any age. A child shorter than others of similar age and gender may be GH deficient. GH deficiency in adulthood may lead to increased body fat and elevated blood sugar level. These deficiencies may be caused by genetic mutations or pituitary damage.
Gigantism occurs when too much GH is released by the pituitary prior to puberty. Excessive GH causes abnormal tallness. If the condition is untreated, the person will continue to grow.
Acromegaly occurs when excessive GH is released by the pituitary. Adults will not grow taller but may notice shoes or rings no longer fit because bones in the hands and feet increase in diameter. A pituitary tumor, or adenoma, may be responsible for excessive GH. Acromegaly may take years to be properly identified as symptoms develop over time. If left untreated, the person’s lifespan may be shortened.
The first indication of a GH disorder may occur when a child starts school and is surrounded by others of similar age and gender that are shorter or taller. During a healthcare visit, height is measured and plotted on a growth chart. If the child is shorter or taller than expected, testing may be ordered.
GH levels are typically highest during sleep and after meals in healthy people. A single GH measurement is rarely useful due to variability in a 24-hour period. Multiple samples at different time points are required to determine GH changes to aid the clinician in making a correct diagnosis.
IGF-I is a hormone produced primarily by the liver in response to GH to promote bone and tissue growth. IGF-I levels are more consistent throughout the day than GH, making IGF-I the best measure of GH status.
To measure IGF-I, a small amount of blood is collected and processed to give serum or plasma. Either can be used in an IGF-I immunoassay. IGF-I immunoassays use antibodies that specifically and selectively bind IGF-I. There are different ways of quantifying IGF-I. The first IGF-I immunoassays used radioactivity, called radioimmunoassays. The next immunoassays used colorimetric determinations, known as enzyme immunoassays. The intensity of color in the sample rather than the amount of radioactivity was measured. The third generation of immunoassays use luminescence (light generation) to measure IGF-I presence and are named chemiluminescence immunoassays. All are still used today.
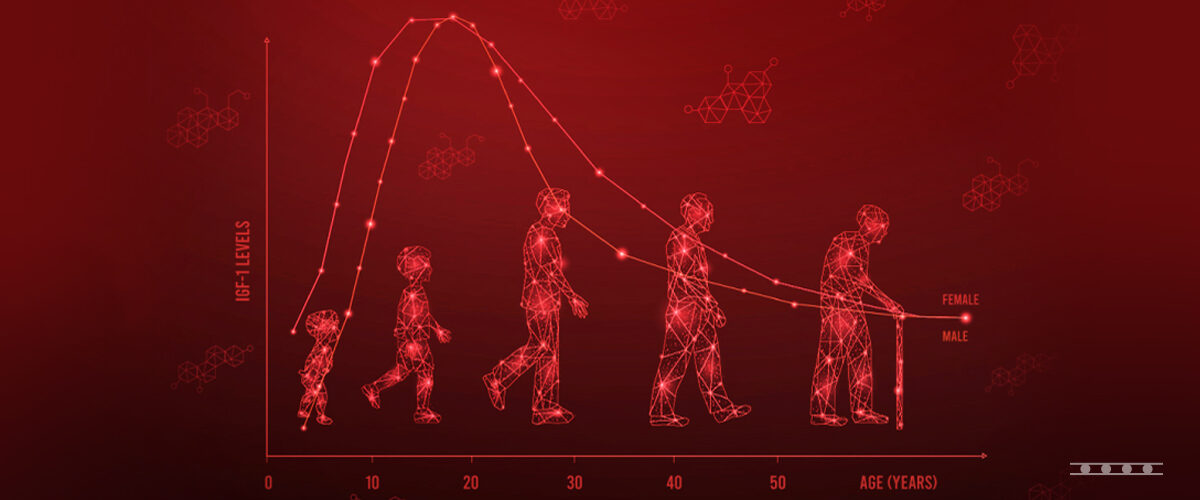
Immunoassay results are compared with values from age and gender-matched reference ranges to determine if IGF-I level is low, normal or high. Low IGF-I may indicate growth hormone deficiency. High IGF-I may result from excess growth hormone. More testing may be required to determine appropriate treatment.
A sample that is collected or stored improperly may cause inaccurate IGF-I result. Some people have antibodies or other compounds in their blood that cause interferences.
IGF-I circulates bound to insulin-like growth factor binding protein (IGFBP). IGF-I is separated from IGFBP to get an accurate measurement. The gold standard is acid chromatography. The serum or plasma is added to an acidic sizing column. Larger compounds (IGFBP-3) move more quickly than smaller ones (IGF-I). IGF-I is about a fifth of the mass of IGFBP-3. Acid column chromatography is very tedious and cannot be used for many samples at a time. Most assays now use acidification pretreatment (separate IGF-I from IGFBP) followed by IGF-II addition. IGF-II binds IGFBP when the sample pH is neutralized prior to immunoassay leaving IGF-I free for measurement without interference from IGFBP or IGF-II.
IGF-I levels rise until puberty and then decline with increasing age. As values from a sample are compared to age and gender-matched individuals, it is essential that reference intervals be appropriate to determine “normal” from low or high values.
Children go through puberty at different ages. This makes it difficult to know if an IGF-I level is low, normal, or high. The clinician determines the child’s physiological age (Tanner Stage) based on physical characteristics to compare IGF-I level with children of the same gender and Tanner Stage.
There is much to be learned about IGF-I as IGF-I has many functions in the body. These are interesting areas that will keep researchers busy making new discoveries about how hormones function for years to come.