Invasive Aspergillosis
The most common Aspergillus species that affect humans are A. fumigatus, A. flavus, A. terreus, and A. niger.1 Aspergillus species are fungi found both indoors and outdoors, particularly in soil, humid walls, and other oxygen-rich environments where they grow as molds on these surfaces.1,2 Aspergillus enters the body when you breathe these spores in and is generally found in the lungs and sinuses.3 These spores can be found in areas of your home where there is dust, carpeting, air conditioning or heating ducts, and even in dried fish and marijuana.3
Most people with functioning immune systems have the ability to “defend” themselves from any potential Aspergillus infection despite breathing in these spores regularly. Thanks to our bodies’ ability to recognize these “dangerous” cues, the spores are contained and don’t lead to any severe consequences. Unfortunately, individuals with weakened or compromised immune systems don’t have the ability to fight off this fungus. This allows Aspergillus to attack the lungs, and potentially spread throughout the body.3
Invasive Aspergillosis (IA) is an infection caused by Aspergillus. IA is most commonly observed in patients with a weakened immune system such as patients with stem cell transplants, solid organ tumors, blood cell cancers, HIV, lung disease, or treated with particular drugs that suppress the immune system (i.e., glucocorticoids).1,2 IA is accompanied by unspecific symptoms including cough, fever, chest pain, or wheezing.4 It is one of the most commonly under-detected diagnoses in ICU patients.5
Aspergillus infections are growing in number and is considered the leading cause of death by invasive fungal infections in the United States, as of 2018.3 In particular, hospitalizations related to IA in the United States have increased 3% per year from 2000-2013.6 In 2014, these hospitalizations led to an estimated cost of $1.2 billion.6 In a study that looked at autopsies of ICU patients, IA was in the top 4 of most common diagnoses likely to lead to death.5 This is why knowing what diagnostic tests are available and being able to diagnose IA early on is critical for management and treatment.
Sample Types Used in Testing for Aspergillus
A key aspect of diagnosing invasive aspergillosis and detecting specific Aspergillus species is to select the proper sample type. Laboratorians should choose high-quality specimens to reduce inaccurate results and aid in precise diagnoses. The most commonly used specimens collected are blood (serum) and respiratory tract fluids such as bronchoalveolar lavage (BAL), sputum, or tracheal aspirate.1
Blood is a sterile sample which means there is a low chance of the sample being contaminated and leading to inaccurate results. Therefore, if Aspergillus was detected in a blood sample, the patient likely has IA.7 On the other hand, lower respiratory tract fluids (i.e., BAL) are more susceptible to contamination. Aspergillus can colonize in the lungs and still not lead to an infection.7 This happens 36-91% of the time, and particularly in patients with chronic lung diseases.7 Hence, it is crucial that the collection procedure is done in a sterile environment so physicians can be confident that a positive test result means there is an actual infection. Alternatively, blood is a suitable non-invasive, in-expensive sample type for detecting Aspergillosis.
Available Diagnostic Methods
There are three main categories of Aspergillus diagnostic tests: conventional diagnostics, immunodiagnostics, and molecular diagnostics.1
Conventional Diagnostics
Conventional diagnostic methods allude to culture tests, microscopy using staining and visualizing techniques, and histopathology. Culture is the most widely available method of diagnosis and most Aspergillus species grow at a rapid pace, within 48 hours.1 Cultures also allow for antifungal susceptibility testing which can help guide clinicians on which antifungal medication will be the most effective (sensitive) or least effective (resistant) for you.1 The main downside of cultures is that it isn’t easy to differentiate when Aspergillus is colonizing the body vs. infecting the body. It takes an expert to be able to make this differentiation and determine which species of Aspergillus it actually is. Additionally, cultures can sometimes be negative and miss the infection.3 On the other hand, microscopy allows for directly examining of the specimen. After the sample is stained with fluorescent dyes, the specimen can be observed under a microscope.1 This can be done in 2-4 hours allowing for swift results.1 However, due to the complexity of these patterns, it could be difficult to distinguish among the various Aspergillus species. Histopathology is another method using a microscope to determine whether Aspergillus is invading the tissues or not.1 The turnaround time is typically 2-3 days, but can aid in detecting IA.1
Immunodiagnostics
The second category of diagnostic tests for Aspergillus is immunodiagnostics. Immunodiagnostics is a method that detects antigens or antibodies that are specific to a particular pathogen and bind to the foreign antigen of interest. For Aspergillus, common antigens of interest include galactomannan, beta-D-glucan, and more recently, galactomannoprotein. Both galactomannan and beta-D-glucan are found in the cell wall of Aspergillus. Galactomannan can be detected with serum or BAL using enzyme-linked immunosorbent assay (ELISA) or lateral flow assay (LFA) tests. These tests are widely available, easy to use, and fairly inexpensive. Galactomannan is useful for early detection of IA and has shown pooled sensitivities (true positive) and specificities (true negative) of proven IA at 71% and 89%, respectively, with the ELISA method.8 The LFA tests are rapid point-of-care tests that can detect invasion of Aspergillus in the body.1 The sensitivities and specificities were 90% and 84%, respectively.1 As, previously stated, beta-D-glucan is also found in the cell wall of Aspergillus, however, this fungal antigen is not specific to Aspergillus and can be found in other fungi.1 Therefore, false positives may arise from exposure to other fungi, antibiotics, or contaminated samples.1
Another antigen that is gaining status is the galactomannoprotein. Galactomannoprotein is a protein also found in the cell wall of different Aspergillus species.2 Like galactomannan, it can be detected with serum or BAL on the ELISA platform.2 EUROIMMUN’s Aspergillus Antigen ELISA shows similar high sensitivities and specifies when compared to another commercially available test.2 This test can be used for both screening and monitoring of patients with IA with the ability to evaluate results semi-quantitatively or quantitatively depending on the laboratorian’s preference.2
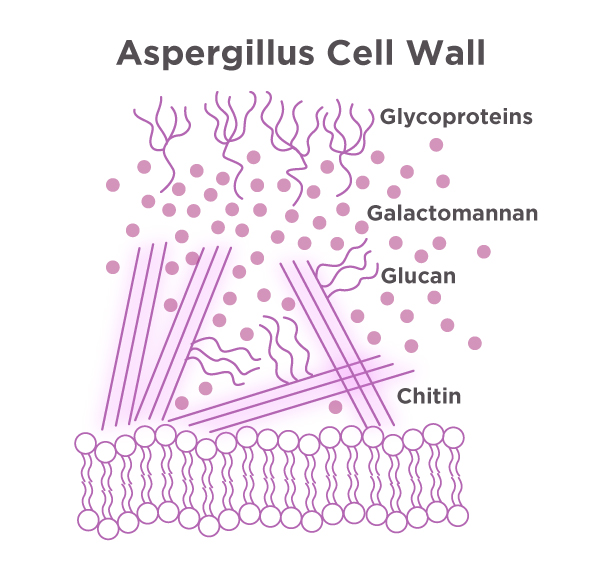
Figure 1. Galactomannan and glycoproteins are found in the cell was of Aspergillus. They can be detected with serum or BAL on the ELISA platform.
Molecular Diagnostics
An example of a molecular diagnostic test is polymerase chain reaction, or PCR. This method allows for rapid detection of Aspergillus using either serum or BAL fluid.1 Although this type of test can be useful, there isn’t a standardized protocol to follow across all laboratories. In the EORTC/MSG criteria revised and updated in 2020, PCR methods are now considered a robust test for screening and confirmation of Aspergillus infection.10 However, the Infectious Disease Society of America did not recommend PCR for detection of Aspergillus in the 2016 guidelines.9
Another molecular test that is not often used is next-generation sequencing, or NGS. Although this test is considered highly accurate and rapid1, it is rather expensive. The main disadvantage of this test is that there isn’t a comprehensive reference genome sequence database available yet.
How can IA be prevented?
Although it is nearly impossible to avoid being exposed to Aspergillus, you can still take precautions to reduce the risk of infection – especially if you have a weaker immune system. For instance, try staying away from places where you will likely encounter a lot of dust or mold, such as construction sites, gardens, and grain stores.11 If you can’t avoid these areas, wearing a mask that filters spores (i.e., N95) can be helpful.11 Furthermore, avoid smoking marijuana and changing your pillowcase regularly can reduce your risk of Aspergillus infection. If you are in a higher risk category for developing IA, your doctor may prescribe antifungal medication to aid in prevention.11
Key Takeaways
Invasive Aspergillosis is an infection caused by Aspergillus species. This is a common fungus/mold that is found oxygen-rich areas. People with weakened immune systems or lung diseases are at a higher risk of developing IA. If your healthcare providers suspect Aspergillus in your lungs, they might collect a serum or BAL sample to test in a laboratory. Because symptoms are not specific, it is important to know which diagnostic tests can aid in early detection and management of IA.
References
- John Z. Deng BDHC, BSc, MSc; Jeffrey D. Klausner, MD, MPH. Review of laboratory diagnostic tests for invasive aspergillosis. In. Medical Laboratory Observer. Vol 53. Website/Print2021.
- Rosenstock P. New ELISA for diagnostics of Aspergillus infections. https://www.euroimmunblog.com/new-elisa-for-diagnostics-of-aspergillus-infections/. Published 2019. Accessed April 12, 2021, 2021.
- Society AT. Aspergillosis And The Lungs. Fungal Disease Series Web site. https://www.thoracic.org/patients/patient-resources/resources/aspergillosis.pdf. Published 2018. Updated January 2018. Accessed May 6, 2021, 2021.
- Eloise M Harman M. Aspergillosis. https://emedicine.medscape.com/article/296052-overview. Published 2020. Accessed April 12, 2021.
- Winters B, Custer J, Galvagno SM, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Quality & Safety. 2012;21(11):894-902.
- Prevention CfDCa. Aspergillosis Statistics. Fungal Diseases Web site. https://www.cdc.gov/fungal/diseases/aspergillosis/statistics.html. Published 2019. Updated December 5, 2019. Accessed April 19, 2021, 2021.
- Tashiro T, Izumikawa K, Tashiro M, et al. Diagnostic significance of Aspergillus species isolated from respiratory samples in an adult pneumology ward. Medical Mycology. 2011;49(6):581-587.
- Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006;42(10):1417-1427.
- Thomas F. Patterson GRT, III, David W. Denning, Jay A. Fishman, Susan Hadley, Raoul Herbrecht, Dimitrios P. Kontoyiannis, Kieren A. Marr, Vicki A. Morrison, M. Hong Nguyen, Brahm H. Segal, William J. Steinbach, David A. Stevens, Thomas J. Walsh, John R. Wingard, Jo-Anne H. Young, John E. Bennett. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. In: IDSA, ed. Clinical Infectious Diseases2016.
- Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clinical Infectious Diseases. 2019;71(6):1367-1376.
- NHS APCSpbt. How can I reduce the risk of Aspergillus Infection? In: Centre NA, ed2015.